Overview
Pancreatitis is inflammation in the pancreas. The pancreas is a long, flat gland that sits tucked in the upper abdomen behind the stomach. The pancreas contains enzymes that aid digestion and hormones that help regulate how the body processes sugar (glucose).
Pancreatitis can occur as acute pancreatitis, which means it happens abruptly and lasts for days. Or pancreatitis can occur as chronic pancreatitis that persists over several years.
Minor cases of pancreatitis can go away without treatment but serious cases may cause life-threatening complications.
Symptoms of Pancreatitis
The patient may usually feel a sudden onset of pain in the middle of the upper abdomen, below the breastbone (sternum).
The discomfort is rarely first felt in the lower abdomen. It will gradually become more intense until it is a constant ache.
The ache may intensify further and become severe. It also spreads into the back in around half of the cases. Eating may exacerbate the pain.
Gallstones result to occur pancreatitis can form very quickly. The signs grow more gradually, over a period of days, when triggered by alcohol.
Leaning forward or taking a fetal position (curling up) will help to somewhat relieve the discomfort. Anyone suffering from persistent pain should seek medical attention.
The following symptoms may also be present:
- Vomiting
- Nausea
- Diarrhea
- Loss of appetite
- Rapid pulse
- Pain with coughing, vigorous movements, and deep breathing
- Tenderness when the abdomen is touched
- Fever and a temperature of at least 100.4 °f (38 °c)
- Jaundice, when the skin and whites of the eyes take on a yellowish tinge
- Does not relieve pain even with strong pain relievers
- Blood pressure can drop or increase, but when the patient is standing it can fall, often causing faintness
When to your doctor
You call your doctor about pancreatitis when:
- You think you may have pancreatitis. People with acute pancreatitis need to get immediate attention to prevent complications that are serious, potentially life-threatening.
- Weight loss continues after pancreatitis diagnosis. You can have a complication which prevents the body from digesting food properly,
- You are pale, cold, have a rapid heartbeat, or are breathing rapidly. You may be in shock and require emergency medical treatment.
- After diagnosis you have chronic pain or diarrhea. You may have chronic pancreatitis or a complication of acute pancreatitis such as a pseudocyst.
Causes
Acute and chronic pancreatitis shares many of the same causes. These include:
- Gallstones
- Drinking a lot of alcohol
- Some medications
- Pancreatic cancer
- Abdominal surgery
- Infections
- Cystic fibrosis
- Injury to your belly
High calcium levels or high triglycerides levels (a form of fat) in the blood may also cause chronic pancreatitis.
Gallstones are the predominant cause of acute pancreatitis. Gallstones are tiny, solid masses which form from bile, a fluid that helps with digestion.
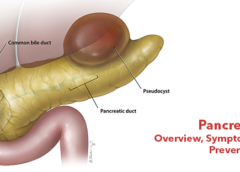
A sufficiently large gallstone can get stuck at the junction where the main pancreatic duct and the common bile duct meet. These ducts drain into the duodenum, the small intestine’s first section.
The pancreas duct carries pancreatic digestive enzymes. The normal bile duct carries bile from the liver and gallbladder or other substances. A stuck gallstone can cause these substances to be backed up, which can lead to inflammation in both the common bile duct and the pancreas.
Risk factors
Factors that increase your risk of pancreatitis include:
Excessive Alcohol Consumption: Research shows heavy consumers of alcohol (people who intake four to five drinks a day) are at increased risk of pancreatitis.
Cigarette Smoking: Smokers are three times more likely to develop chronic pancreatitis than non-smokers, on average. The good news is that quitting smoking reduces the risk by about half
Obesity: If you are obese you are more likely to develop pancreatitis
Family History of Pancreatitis: In chronic pancreatitis, the role of genetics is increasingly recognized. If you have family members with the disorder, your risks increase — especially when combined with other risk factors.
Complications
Pancreatitis can have severe complications, including:
- Diabetes if damages insulin-producing cells
- Infection of your pancreas
- Kidney failure
- Malnutrition if your body can not get adequate nutrients from the food you eat due to a lack of digestive enzymes
- Pancreatic cancer
- Pancreatic necrosis when tissues die because there is not enough blood in your pancreas
- Breathing problems when chemical changes in your body are affecting your lungs
- Pseudocysts, when fluid collects in pockets on your pancreas. They can burst and become infected.
Prevention
Pancreatitis may not be preventable, depending on the cause. Still, there are many things you can do to lower the risk:
- Limit your alcoholic drinks.
- Stop smoking.
- Maintain a healthy weight.
- Eat a balanced diet.
Eating high-fibre foods and avoiding sugar can help you prevent gallstones, which are the leading cause of acute pancreatitis.
Leave a Reply
You must be logged in to post a comment.