Nearly 0.5% of the world’s adult population suffers from Rheumatoid arthritis (RA)- an autoimmune disease that attacks the joints, usually many joints at once. The disorder is much more common in women and highly prevalent in adults over 40.
In this blog, we shall be discussing Rheumatoid arthritis causes, symptoms, and diagnosis techniques. We hope this blog will help people with RA better understand the disease and get the best treatment possible.
Rheumatoid Arthritis Fast Facts
- About 75% of RA patients are women
- 3% of women may get rheumatoid arthritis in their lifetime
- Most common among adults (age 30-50 years)
- RA-related disabilities can lead to early retirement
- Severe or untreated RA reduces life expectancy by 6-10 years
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is an autoimmune and inflammatory disease in which your immune system starts attacking healthy cells in your body. The body’s natural defense mechanism cannot distinguish between healthy cells and foreign ones, causing inflammation (painful swelling). RA is predominantly a joint disease that simultaneously affects multiple joints.
What Causes Rheumatoid Arthritis?
Our immune system uses inflammation to fight foreign invaders in our bodies, such as bacteria and viruses. When you have an autoimmune disease, your immune system accidentally causes inflammation in healthy tissue.
The immune system in a healthy person is dormant (inactive). The immune system gets activated when the body is infected.
The immune system turns overactive in people with an autoimmune disorder, causing inflammation even when there is no infection. In cases like rheumatoid arthritis, inflammation occurs around the body’s joints, resulting in joint swelling and pain that rheumatoid arthritis patients experience.
Unfortunately, researchers have not yet identified the exact rheumatoid arthritis causes. However, medical professionals identify specific RA risk factors. These include:
1. Sex
RA is twice as common in women than in men. Women’s estrogen levels drop during menopause which may have a role in the increased risk of arthritis.
2. Age
RA can strike at any age, but it is most frequent among adults (30-50 years). RA treatment needs in adults are different from children and young.
3. Family History
A positive family history of rheumatoid arthritis puts one at a slightly higher risk. Some believe that smoking increases the incidence of autoimmunity, whereas others believe that environmental factors such as past viral infection play a role.
4. Smoking
Smoking is a risk factor for RA. Smoking increases cytokine count and puts the body under extreme stress, causing inflammation.
5. Medication
Interferon-alpha, a medicine used to treat hepatitis, autoimmune illnesses, and other conditions, has been linked to RA.
Common Symptoms for Rheumatoid Arthritis
The disease often begins slowly. Early Rheumatoid Arthritis symptoms may include:
- Minor joint pain
- Stiffness
- Fatigue
Joint symptoms may include:
- Feel achy and stiff in the morning
- Stiffness after rest or inactivity
- Inflamed or swollen
- Joint pain on both sides of the body.
- Tender or warm
- Loss of mobility and deformation
Other symptoms include:
- Pain in the chest
- Dry mouth
- Burning and itching sensation in eyes
- Small, round lumps under the skin
- Tingling or a burning sensation in hands and feet
- Sleep difficulties
RA almost always affects your joints. The smaller joints, such as your fingers and toes, are the first to show signs of RA. Wrists, ankles, knees, elbows, hips, and other joints will be affected as the condition progresses.
The severity of RA symptoms varies, and they might come and go. If under-treated or ignored, inflammation from RA can cause joints to distort and shift out of place.
How is Rheumatoid Arthritis Diagnosed?
The preliminary steps include a thorough physical examination of the affected parts. Joints are closely examined for signs of swelling, redness, or impaired reflexes. Your doctor will also want to know when and how your Rheumatoid Arthritis symptoms started. If you experienced any flare-ups or improvements in symptoms recently?
The information helps you and your provider figure out the RA severity and causes. Rheumatoid Arthritis symptoms can be misgiving, making diagnosis more challenging. Symptoms of viral infections can be mistaken for those of RA. After a preliminary examination, your doctor will suggest blood and imaging tests. No test can definitively determine whether or not patients have RA. The majority of RA patients will have some abnormal test results.
The following are two lab tests that are usually positive in most RA patients and can aid with the diagnosis:
- Rheumatoid factor
- Anti-CCP antibody
Secondary RA tests include:
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Antinuclear antibody
- Joint fluid analysis
Joint X-rays can assist in detecting RA, but they may not be too suggestive in the early stages of the disease. Even if the initial X-rays are normal, they are crucial to determine the progress of the disease during a later stage. MRI scanning may also be prescribed to confirm or evaluate the severity of RA.
How Is Rheumatoid Arthritis Treated?
Most cases of rheumatoid arthritis (RA) require long-term management by a rheumatologist or arthritis specialist. Treatment typically involves medications, physical therapy, exercise, education about RA, and, if needed, surgery.
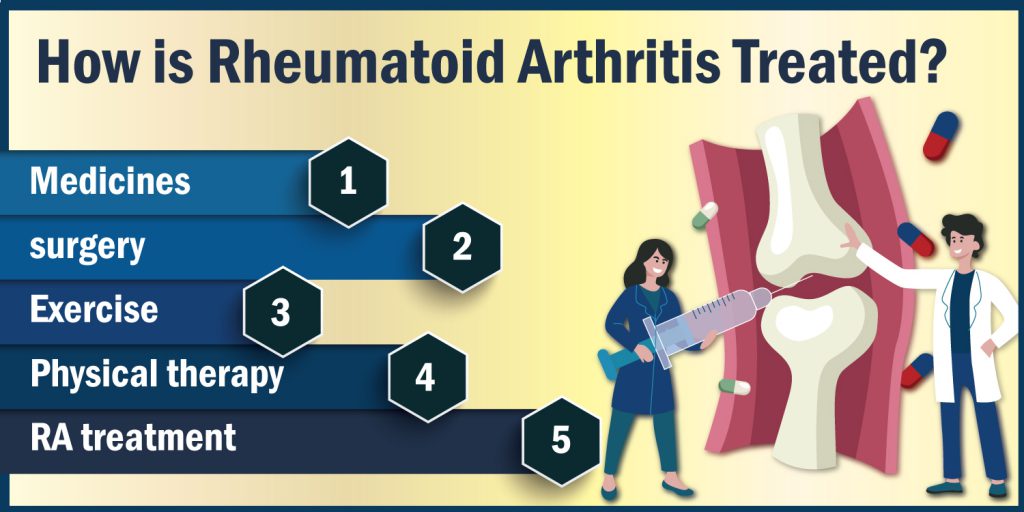
1. Medicines
The drugs commonly prescribed for rheumatoid arthritis (RA) include anti-inflammatory and nonsteroidal medications, such as aspirin, ibuprofen, naproxen, and celecoxib. These medications help reduce joint swelling and inflammation. They are often used in combination with disease-modifying antirheumatic drugs (DMARDs) to help prevent joint damage.
2. Surgery
In severe cases, the provider might suggest Rheumatoid Arthritis surgery –Synovectomy (removal of the joint lining). Surgery reduces pain and improves joint mobility and function. The doctor may also suggest a total joint replacement, total knee replacement (TKR), and hip replacement.
Living with Rheumatoid Arthritis
Unfortunately, to date, there is no permanent cure for RA. However, those at higher risk can do some simple things to cope with the disease.
- Maintain a healthy diet.
- Maintain your fitness by exercising.
- Make it a habit to do pranayama and yoga every day.
- Make sure you get enough sunlight to maintain healthy Vitamin D levels.
All of these will assist the body in dealing with discomfort and slow the progression of the disease.
It’s good to stay physically active most of the time, but when the disease flares up, you should reduce your activities. Rest is generally beneficial when a joint is inflamed or when you are weary.
Do not overstress your body. Follow a low-impact regular exercise routine, such as stretching, at these times. It will boost overall health and relieve joint pressure.
Low-impact workouts are recommended for RA patients to improve muscular strength and maintain the joint’s flexibility.
The Bottomline
Although RA is a serious illness, it can be controlled with medication and a healthy lifestyle. To avoid major issues, Rheumatoid Arthritis symptoms must be identified and treated as soon as possible. You should consult your doctor if you experience joint discomfort, pain, stiffness, or swelling that has persisted for more than a few months.
A physical or occupational therapist can assist you in determining which activities are appropriate for you and at what level or pace you should participate in them. Find the best Rheumatoid Arthritis specialists near you with Kayawell-an online platform that connects patients and providers instantly.
Leave a Reply
You must be logged in to post a comment.