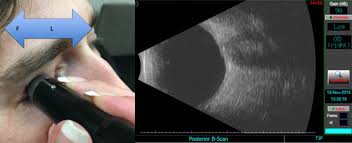
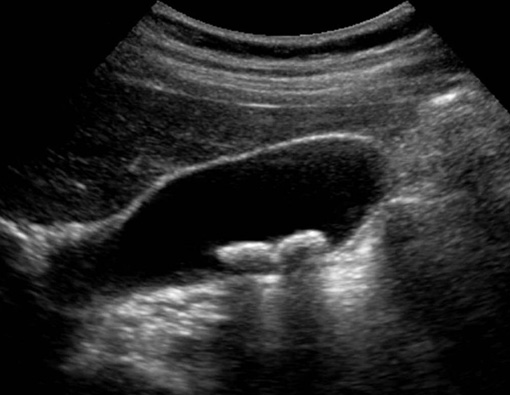
Although it is a relatively rare disease, primarily found in the Caucasian population, uveal melanoma is the most common primary intraocular tumor in adults with a mean age-adjusted incidence of 5.1 cases per million per year. Tumors are located either in iris (4%), ciliary body (6%), or choroid (90%). The host susceptibility factors for uveal melanoma include fair skin, light eye color, inability to tan, ocular or oculodermal melanocytosis, cutaneous or iris or choroidal nevus, and BRCA1-associated protein 1 mutation. Currently, the most widely used first-line treatment options for this malignancy are resection, radiation therapy, and enucleation. There are two main types of radiation therapy: plaque brachytherapy (iodine-125, ruthenium-106, or palladium-103, or cobalt-60) and teletherapy (proton beam, helium ion, or stereotactic radiosurgery using cyber knife, gamma knife, or linear accelerator). The alternative to radiation is enucleation. Although these therapies achieve satisfactory local disease control, long-term survival rate for patients with uveal melanoma remains guarded, with risk for liver metastasis. There have been advances in early diagnosis over the past few years, and with the hope survival rates could improve as smaller tumors are treated. As in many other cancer indications, both early detection and early treatment could be critical for a positive long-term survival outcome in uveal melanoma. These observations call attention to an unmet medical need for the early treatment of small melanocytic lesions or small melanomas in the eye to achieve local disease control and vision preservation with the possibility to prevent metastases and improve overall patient survival.


 Contact Us
Contact Us

 Hospitals
Hospitals
 Doctors
Doctors
 Diagnostic
Diagnostic
 Pharmacy
Pharmacy
 Health Tips
Health Tips
 Blog
Blog